Everyday tasks such as remembering to turn off the stove or finding your way to the grocery store appear mundane but can be dangerous if forgotten. When it comes to dementia, such mundanities are oftentimes impossible feats. Dementia is an age-old condition prevalent among the elderly and typified by a gradual decline in memory and reasoning. It is a debilitating condition that affects over 40 million people worldwide. Worst of all, most treatments available are unable to reverse the disease once it develops. Clearly, there is an urgent need to approach this problem from new angles. In early 2021, scientists at Stanford University School of Medicine unveiled an innovative approach toward correcting dementia by manipulating the immune system.
Prostaglandins and macrophages
These scientists specifically focused on 2 components of our immune system: prostaglandins and macrophages, neither of which are traditionally associated with brain function. Prostaglandins are molecules of fat that allow us to feel pain and fever. Anytime we take an aspirin, we are essentially blocking prostaglandins from causing such discomforts. Macrophages, on the other hand, are a type of immune cell generally considered to be the “vacuum cleaners” of our body. They literally eat and digest microscopic debris or organisms that can cause harm if left uncleansed.
Importantly, macrophages and prostaglandins interact to control a process known as inflammation, a multifaceted condition that alerts the body to infection. Recently, this process has been increasingly recognized as a contributor to dementia. Long-term inflammation creates an environment that is toxic to brain cells, also known as neurons; and when enough neurons die, brain networks that help maintain new memories become unstable. The result? Dementia.
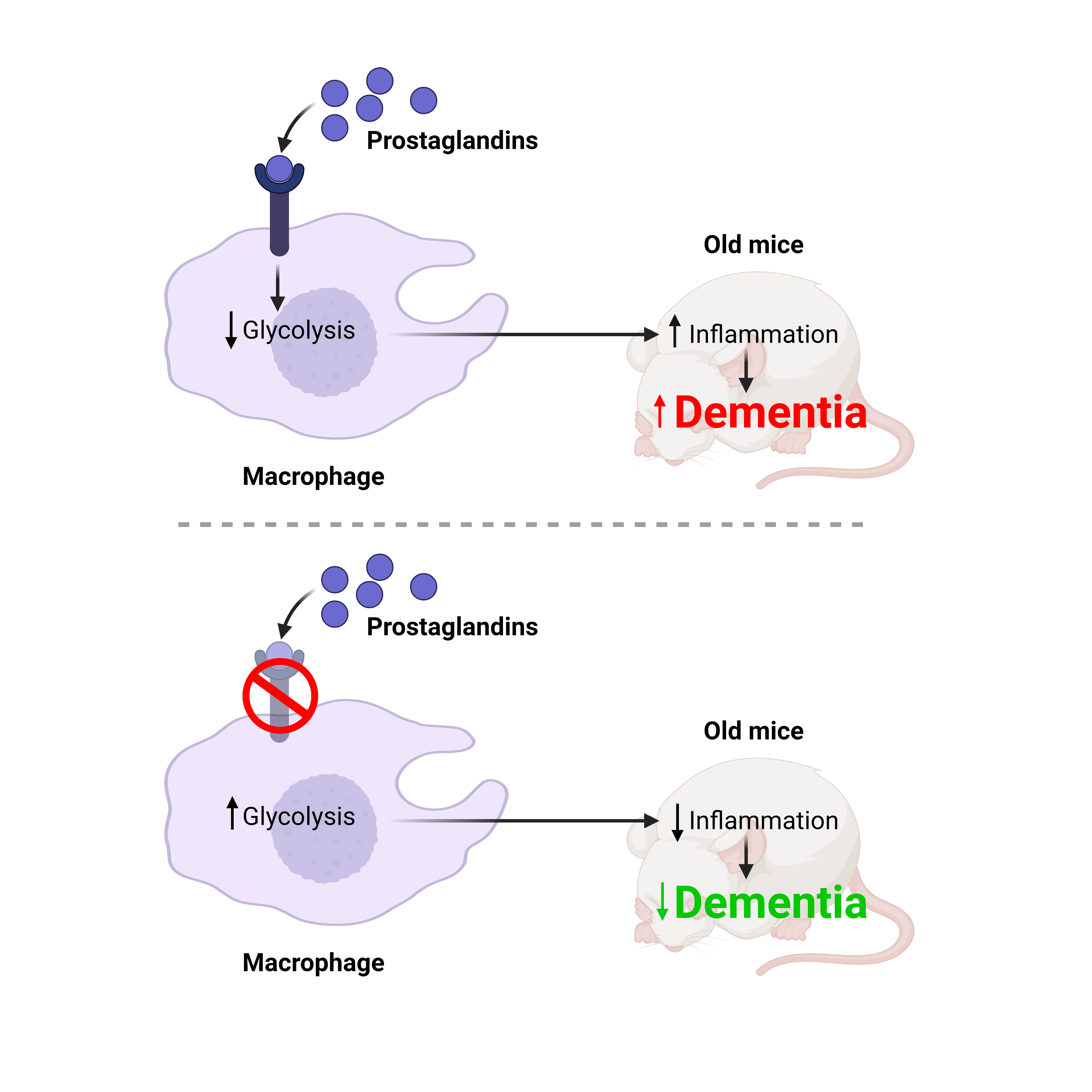
In this study, scientists reasoned that altering the bond between macrophages and prostaglandins may substantially counteract this inflammatory mechanism of damaging the brain in dementia patients.
Dementia-resistant mice
First, the researchers wanted to find out if blinding macrophages to prostaglandins will improve dementia. To do this, they focused on mice, which typically develop cognitive decline upon reaching old age. Specifically, they created “mutant” mice whose macrophages have genetically lost the protein needed to cooperate with prostaglandins. The researchers were astonished to discover that upon old age, these “mutant” mice were resistant to developing age-associated dementia. In fact, they retained the cognitive wherewithal of mice that were 8 times their junior.
One test they used to assess cognition is known as the Barnes maze task, wherein mice are taught to escape a “maze.” Young mice with normal memory will quickly learn how to escape whereas old mice with memory deficits will take longer time. Interestingly, the “mutant” mice, despite reaching old age, learned to escape just as quickly as the young healthy mice.
Beyond testing memory behavior, the researchers also measured memory formation by focusing directly on microscopic brain cells, or neurons. To do this, they used metal probes to test how well neurons electrically communicate in the hippocampus, the region of the brain conventionally associated with learning and memory. Typically, neuron-to-neuron communication is robust in young healthy mice but weakened in elderly mice with memory issues. Amazingly, the hippocampal neurons of the “mutant” mice were able to maintain strong communication despite reaching old age.
Overall, these findings suggest that the interaction between prostaglandins and macrophages promotes the development of dementia.
Prostaglandins change how macrophages process sugar
The scientists next wanted to understand how prostaglandins directly affect macrophages. They took macrophages from regular mice and bathed them in a pool of prostaglandins. This led to a fundamental shift in how these macrophages consume sugar ‒ namely, glucose. Specifically, prostaglandins dialed down a process known as glycolysis, which controls how glucose molecules are broken down and siphoned for energy. Through many mechanisms, changes in sugar processing can fundamentally change a cell’s function ‒ and in the case of macrophages, the decrease in glycolysis led to functions that promoted inflammation. Over the life of a mouse, such inflammation can encourage the type of neurodegeneration seen in dementia.
Taking a step away from mice, the researchers also wanted to know if human macrophages share the same reaction to prostaglandins as in mice. They isolated human macrophages from patient blood samples and again, found that prostaglandins reduced glycolysis. Moreover, when scientists compared macrophages from old versus young patients, they noticed that with age, macrophages appear to increase the level of their prostaglandin receptor proteins. This suggests that macrophages are more susceptible to the influence of prostaglandins in the elderly, who are more prone to developing memory deficits. All in all, these findings provide some confidence that the prostaglandin-macrophage-relationship also promotes dementia in humans as it does in mice.
The aspirin for dementia?
So far, the researchers have shown that macrophages & prostaglandins work together to encourage dementia. An integral question then remains to be answered: Can blocking prostaglandins be a useful new strategy for treating dementia?
To address this possibility, the researchers performed a simple experiment in regular old mice. For one month, they fed these mice a drug that disrupts the prostaglandin-macrophage interaction. Incredibly, the treatment appeared to significantly reverse the dementia that would have been expected in these mice. In the Barnes maze task, their ability to learn was just as agile as their younger peers. Furthermore, their hippocampal neurons showed robust neural communication and their macrophages showed unaltered sugar processing.
Altogether, these scientists exposed a powerful collaboration between prostaglandins and macrophages in the context of dementia, one that can be potentially manipulated to reverse such a debilitating disease. This is no small feat as dementia is often considered irreversible. Of course, the drug they used requires better characterization before entering clinical trials. Furthermore, other existing drugs may also prove effective, namely those that control the prostaglandin system ‒ many of which share the same biology as the safe and popular pain-reliever, aspirin. Essentially, these scientists have paved the way for a novel and powerful arsenal of pharmacologies with which dementia can be conquered.
This article summarizes work from: Minhas, P.S., Latif-Hernandez, A., McReynolds, M.R. et al. Restoring metabolism of myeloid cells reverses cognitive decline in ageing. Nature 590,122–128 (2021). https://doi.org/10.1038/s41586-020-03160-0
Cover Image: CC BY-NC-ND