Following the emergence of the COVID-19 pandemic, immunology has consistently dominated the headlines of societal conversations. After the first vaccine became available in December 2020, decisions regarding vaccination have been a strong debate for many individuals. With the frequent appearance of new coronavirus variants, including Omicron and Delta, a second challenging decision has arisen of whether a booster jab is necessary.
Vaccines are considered an effective way to manage SARS-CoV-2 (the viral cause of the COVID-19 disease), but recent research from a 2021 study, lead by Tré-Hardy and colleagues, has found a substantial decline in immunity 6 months after the second vaccination. While infection rates remain high and new variants of the virus continue to emerge, this research highlights the importance of booster doses.
How does vaccination work?
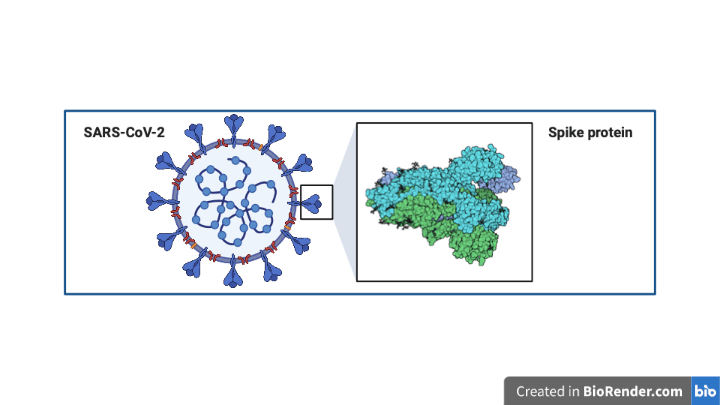
SARS-CoV-2 viruses have characteristic proteins that protrude from their exterior surface called Spike proteins (Figure 1). These Spike proteins are key for the virus to enter human (host) cells, such as those that line the respiratory tract.
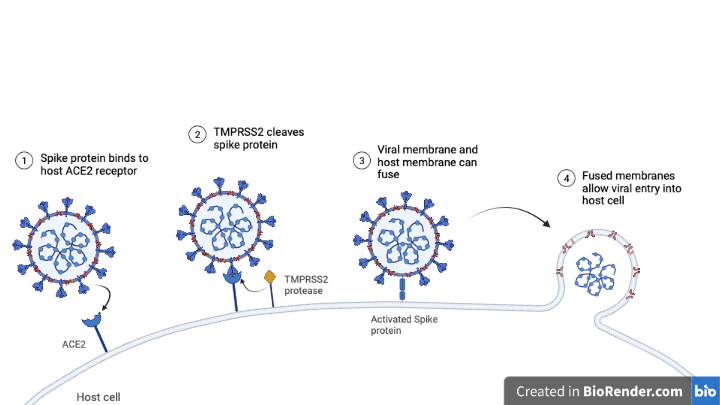
Respiratory tract cells, for their part, have a protein on their cell-surface called ACE2. ACE2 can directly interact with SARS-CoV-2 Spike proteins, providing an anchor point for the virus to latch onto our cells and ultimately get inside. Once the viral Spike protein binds with ACE2, a third protein, termed TMPRSS2, severs the Spike protein. This process enables the viral membrane and respiratory cell membrane to merge, causing infective viral content to spill inside our own cells (Figure 2). Once a virus enters the host cell it can co-opt the host’s protein production mechanisms to produce new viral protein; this is how a virus replicates in order to spread.
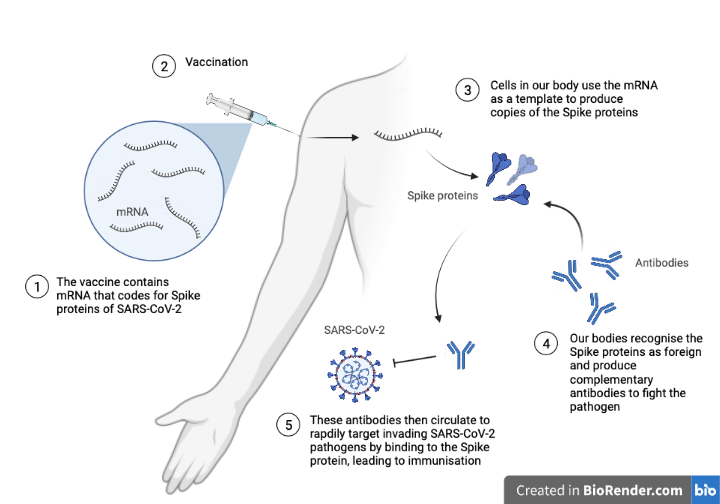
One approach to prevent viral infection is through vaccination. Vaccinations either contain weak or inactive viral parts (antigens), or they contain the instructions to produce these antigens. In the case of the Moderna vaccine, the shot contains mRNA, which is a molecular template for making proteins – in this instance, the SARS-Cov-2 spike protein.
When the vaccine deposits this mRNA into our arms, our cells produce copies of the Spike protein that are then released into circulation (Figure 3). The presence of these proteins within our systems is abnormal, and so they are recognised as foreign by our immune systems. Because this process introduces only a small part of the virus into circulation, which cannot cause infection without the entire viral machinery, vaccination is considered a safe and effective way of preventing future disease.
The detection of foreign proteins by the immune system activates an immune response, producing complementary antibodies to mark the foreign proteins for destruction. Antibodies help to protect the body from invading pathogens; they are produced following vaccination. These antibodies recognize and bind to the Spike proteins and act as little tags, marking their targets for destruction by the immune system. The idea is that, when a vaccinated person breathes in a real SARS-Cov-2 viral particle, the corresponding antibodies will already be present in their bodies to recognize and flag the virus for destruction before it can infect numerous cells and cause severe illness. Two vaccine doses have been shown to effectively establish high levels of anti-SARS-CoV-2 antibodies in recipients, demonstrating the promising effects of managing COVID-19 through vaccinations.
What happens after two vaccine doses?
In the 2021 Belgium study, researchers measured the change of anti-SARS-CoV-2 antibodies in healthcare workers, directed towards the Spike protein, at 5 time points throughout the vaccination process of the first and second dose. The quantification of antibodies was established using antibody titers. Antibody titers enable the level of antibodies in the blood to be determined, which correlates with the degree of protection provided by a vaccine. Blood samples are taken from the individual and serially diluted (a stepwise dilution of the blood using saline). Known amounts of the antigen (Spike protein) are added to the sample to quantify the amount of free antibodies. A high concentration of antibodies corresponds to a larger level of dilution and the results of the test represent the highest dilution level at which no more antibodies can be detected.
The study on healthcare workers demonstrated a significant decrease of antibodies, in both the naïve (people who have not been infected by COVID-19) and previously infected groups, 6 months after the second vaccination dose. Specifically, this drop in antibodies is seen between 3 months and 6 months post-vaccination. Despite this, all participants still had some detectable antibodies, demonstrating the ongoing protection provided by the vaccination.
Is a third dose necessary?
Following the findings of this study on healthcare workers, the researchers suggest that a third booster dose of the Moderna vaccine is necessary to increase levels of circulating antibodies. A higher concentration of circulating antibodies within the blood demonstrates a stronger and quicker immune response to invading SARS-CoV-2 pathogens. The significant drop in antibodies after 6 months suggests a weakened level of immunity. Several confounding factors were also explored in relation to antibody levels (e.g. age, sex, immunodeficiency, BMI, diabetes, cardiovascular disease) but none of these influenced the change in antibody levels. A booster jab may therefore restore antibody levels and maintain greater immunity amongst the population to effectively manage COVID-19.
However, many low-income countries are limited in their supply of COVID-19 vaccines and therefore lack the opportunity to offer a booster jab to every individual. In these restricted populations, it may be beneficial to initially offer the booster jab to the naïve population because this group showed the greater decline in antibodies.
Although there is positive evidence to suggest that a booster dose may help to maintain antibody levels, there are numerous other immune effectors that are important in the fight against SARS-CoV-2 (see further reading below). Nonetheless, with the present evidence provided, a booster jab should be considered wherever possible to maintain higher levels of immunity amongst the population.
Journal Article: Tré-Hardy M, Cupaiolo R, Wilmet A, Antoine-Moussiaux T, Della Vecchia A, Horeanga A, Papleux E, Vekemans M, Beukinga I, Blairon L. Immunogenicity of mRNA-1273 COVID vaccine after 6 months surveillance in health care workers; a third dose is necessary. J Infect. 2021 Nov;83(5):559-564. doi: 10.1016/j.jinf.2021.08.031. Epub 2021 Aug 23. PMID: 34437927; PMCID: PMC8380546.
Further Reading: Chaplin D. D. (2010). Overview of the immune response. The Journal of allergy and clinical immunology, 125(2 Suppl 2), S3–S23. https://doi.org/10.1016/j.jaci.2009.12.980
Cover image courtesy of Gerd Altmann on Pixabay
Is there any truth in the rumour that red wine also has a beneficial effect in keeping up antibody levels , if so could this reduce the need for further booster jabs
LikeLike
Hi Leanord.
Interesting thought! I’m not personally aware of any studies that have explored the direct effects of red wine consumption on antibody production in humans. That being said, there have been many studies exploring the beneficial effects of resveratrol (a compound commonly found in wine) on aspects of human health. Many of these benefits have been linked to improved immune function. Here’s a link to a paper that expands on this topic: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6566902/
I have also come across an interesting study on piglets, that shows significant increases in antibody titers following vaccination when treated with a resveratrol dry suspension (compared with controls): https://www.hindawi.com/journals/ecam/2018/5952707/
In response to your question however, the Moderna vaccine enables our body to produce complementary antibodies against Covid-19 viral particles. This improves our immune response and capability to fight off Covid-19 infection. Red wine would not be able to produce this specific response but, that being said, if we consider the present research available, compounds in wine might improve more generalised aspects of our immune function. I think this is an interesting topic to explore more!
LikeLike